By Kevin Harrison and Alison Paxson

It’s 7:30 am and Sam and his older brother Sean are on their way to their elementary school classrooms. Sam is a first grader and has been crying non-stop since they left their apartment to board the school bus nearly an hour ago. No matter what Sean does, he can’t get his little brother to calm down.
The only way he was able to convince him to get on the bus without a tantrum was to remind him that it was his day to talk to Mr. Rob, a counselor at the school. Sam has been seeing Mr. Rob since the beginning of the school year when it became clear to his first-grade teacher that Sam’s behavior was beyond sadness and attention-seeking. Sam was suffering emotionally and needed help. Sam’s parents were quick to approve the offer for behavioral health services at the school, and also grateful that his classroom teacher confirmed what they had observed over the past year.
Though Sean and Sam are fictional, their situation is very typical and behavioral needs among young children is becoming more and more common in our schools.
Prior to 2020, youth throughout Ohio experienced the aftermath of the opioid epidemic, high rates of trauma and an increasing uninsured rate amongst children, leading to behavioral health challenges that have been further exacerbated by the COVID-19 pandemic. At a time when so many young Ohioans are struggling, it is critical that the state build a network of behavioral health services to provide timely, quality care to all children, regardless of income or location.
Key Statistics
In 2022, a national survey of parents found that 75% thought their child would benefit from mental health counseling, up from 68% the year before.
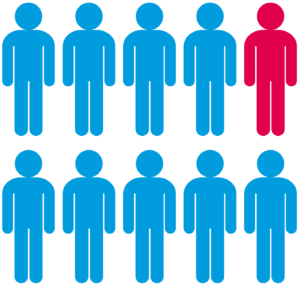
In 2020, nearly one in eight Ohio children received a diagnosis of anxiety, depression or both, up 42% from 2016 – the 10th-highest increase nationwide.
In 2022, 60% of LGBTQ youth surveyed by The Trevor Project wanted mental health care in the past year but could not access it.
Source: 2022 Kids Count® Data Book
Behavioral health services for youth span the continuum of care from early identification and diagnosis, prevention education to intervention and counseling. However, families throughout Ohio face challenges in getting care for their children – which include a lack of providers, lack of insurance coverage and other barriers, such as unreliable transportation or lack of public transportation, lack of paid time off and lack of knowledge about behavioral health in general.
One in 10 Ohio children miss more than seven days of school each year due to illness or injury.
Source: 2019-2020 National Survey of Children’s Health Resources and Services Administration
Untreated health issues, including behavioral health conditions, contribute to high rates of chronic absenteeism among children throughout the state. One in 10 Ohio children miss more than seven days of school each year due to illness or injury. Chronic absenteeism is directly related to poor academic performance and puts a child at risk of academic failure and lifetime challenges in terms of financial stability and quality of life – including poor health.
How are school districts addressing behavioral health challenges?
According to the 2019-20 National Survey of Children’s Health, only about 52.7% of school-age children who have received a behavioral health diagnosis are receiving services. This excludes the many children who potentially have behavioral health needs yet lack a diagnosis. Parents and teachers recognize the challenges children are experiencing and can support behavioral supports, but behavioral health professionals are needed to address more significant needs.
Ohio’s funding commitment for children’s behavioral health
The last biennial budget, H.B. 10 – FY 2022-2023, demonstrated a funding commitment in Ohio for children’s behavioral health, including:
- $2 million in funds that directly support behavioral health services in schools grew to include earmarks for behavioral health telehealth services
- Certain categories of the school funding plan allowed to address health and behavioral health services
- Increased investments in early childhood mental health counselors and consultation used to promote identification and intervention for early childhood mental health and to enhance healthy social emotional development to reduce preschool to third grade classroom expulsions
- Funding included to support and expand Ohio’s behavioral health workforce
- $3.6 million allocated to create the Child and Adolescent Behavioral Health Center of Excellence charged with providing technical assistance, training, professional development and more to build behavioral health capacity
- The Ohio Department of Mental Health and Addiction Services provided funding for school districts to also support behavioral health services
Funds are also available to support aspects of behavioral health through targeted funds from the federal and state sources.
District Spotlight: Greene County Education Service Center
Across Greene County, an area impacted by the opioid crisis, school districts reported that many children entering kindergarten were not prepared to learn. Many were presenting with significant behavioral health challenges creating significant barriers to their learning and development. The Greene County Education Service Center (ESC), which had a behavioral health unit for more than 20 years, decided that it was in everyone’s interest to determine how best to provide early intervention services for children and families attending both public and private pre-schools.
The ESC successfully secured a Safe Schools, Healthy Students Grant for $500,000 per year for four years. Through a needs assessment found that children, primarily in the privately operated preschools, they were experiencing high rates of removal due to behavioral issues. It became clear that many programs were not equipped to work with children who had significant trauma and behavioral issues. Greene County ESC used the grant funds to support an early childhood mental health trainer who could support early childhood educators and families. Through strong partnerships with area preschool programs, local Family and Children First Councils, school districts and behavioral health professionals, Greene County ESC is helping to make sure all children are prepared to enter kindergarten with positive behavioral health.
Policy Recommendations
Recommendation 1
In partnership with families, leverage existing federal and state funding to identify both short- and long-term strategies to effectively allocate public funding to meet every student’s behavioral health needs.
- Audit State Health Funding Allocations and Formulas: The state legislature should leverage federal funds to establish a commission to audit student health funding systems to maximize impact through the following strategies:
- Study ways to match local funds in part or in full by state funds
- Determine necessary increases in state funding to ensure districts and community partners are able to adequately meet local student needs
- Identify reporting metrics that should be tied to this increase in funding
- Establish Local Health Reporting and Use: Districts should voluntarily implement reporting requirements that incorporate aggregate health outcomes. Districts should engage with these data to identify clear and immediate needs and leverage federal funding to advance targeted strategies for success.
- Develop Planning Process: A coalition of state and community partners should collaboratively develop a planning process and accompanying resources for districts to identify effective strategies for leveraging public funds for children’s health needs. This effort could be supported in part or in full by federal stimulus funding.
Recommendation 2
Expand the type of services and providers that are allowed to bill Medicaid – through the Medicaid in Schools Program – to provide more students with access to health coverage and services while maintaining a commitment to financial stability.
- Secure Center for Medicare and Medicaid Services Free Care Policy Waiver: The Ohio Department of Medicaid should submit a State Plan Amendment to Center for Medicare and Medicaid Services to allow for school-based health care costs for non-IEP students enrolled in Medicaid to be reimbursed under the Free Care Policy. In 2014, the federal government expanded the opportunity for Medicaid-eligible students without an Individualized Education Plan (IEP) to receive services reimbursed by the Medicaid in Schools Program. At least 16 other states, including Indiana, Michigan and Kentucky, allow Medicaid reimbursement for students without an IEP.
- Allow for Medicaid Administrative Claiming of Family Engagement Activities: Community providers should bill Medicaid for this engagement. The absence of meaningful engagement with community health care providers and families is a barrier to creating a self-sustaining school-based health program. The Ohio Department of Medicaid should leverage the permissibility in Medicaid Administrative Claiming for items that improve the administration of Medicaid services, to compensate providers for spending time on family and community engagement tied to school-based health care needs.
- Incentivize Managed Care Organizations: Managed Care Organizations should use their community investment obligation to pay community-based providers bonuses for meeting state-defined quality metrics that are aligned with state population health goals, including goals for behavioral health and education.
- Encourage Incentivize Managed Care Organizations to Expand Support for Child Services: The Ohio Department of Medicaid already requires its Incentivize Managed Care Organizations (MCO) to offer and address whole child services and Social Determinants of Health, but has the opportunity to encourage further partnerships and flexibility for MCO’s to deepen their financial support of school-based health to cover related services that improve health. Some of those funds could be used to cover the costs of school health that are not funded in other ways.
Recommendation 3
Support districts, communities, parents, families, providers and statewide actors to grow partnerships between school districts and health care providers focused on student behavioral health needs.
- Leverage Holistic Data for Need Identification: Districts and communities should leverage existing data such as the Ohio Healthy Youth Environments Survey or Healthy Student Profiles (housed within the Ohio Department of Education) to identify community health needs and areas where additional partnerships with health care providers may help address gaps. Districts should also create forums for families, students and other community members to discuss health challenges and propose solutions.
- Provide State Technical Support: The Ohio Department of Education and Ohio Department of Health (or consortium approach) should jointly create resources highlighting effective strategies as well as best practices from across the state on how to build effective partnerships between schools and a variety of health care providers.
- Incentivize Community Partnerships: A statewide coalition should craft a plan to jointly create a grant program to encourage the development of local or regional coalitions dedicated to creating partnerships between schools and health care providers to ensure that all children’s needs are met. Applicants should be required to clearly identify strategies for engaging the broader community in feedback loops to ensure local stakeholder needs are considered as well as articulate their metrics for success. The coalition should determine the most appropriate avenue for funding (e.g., state appropriations, federal funding or philanthropic funding).
This resource was co-written by former Senior Manager of Advocacy Kevin Harrison and Alison Paxson, a Senior Policy Associate for the Children’s Defense Fund-Ohio (CDF-Ohio).